Adult ADHD: Medication Plus Cognitive Behavioral Therapy, Latest Research
An article by Sanjay Gupta*, “Talk Therapy Alone for ADHD Doesn’t Cut It,” reviews a recent multi-site study of treatment for Adult Attention Deficit Hyperactivity Disorder [ADHD]. In sum, “talk” therapy does have a significant benefit, but it doesn’t benefit ADHD symptoms quite as much as medication or the combination of medication plus therapy.
Treating ADHD means BOTH
 1) improving symptoms of concentration, focus, and memory with medications AND
1) improving symptoms of concentration, focus, and memory with medications AND
2) developing skills for organization, social behavior, following-through, remembering responsibilities, and anticipating consequences.
The research addressed mainly the symptom domain.
We have known since the 1980s that “psychosocial” therapy, such as individual psychotherapy, group therapy, or social skills training, does not significantly reduce the symptoms of most children with ADHD unless medication is also used. The most common medications for children with ADHD are formulations of one of four drugs,
1) methylphenidate (e.g., Concerta, Daytrona, Focalin, Metadate, Methylin, Ritalin),
2) dextroamphetamine (Adderall, Desoxyn, Vyvanse),
3) atomoxetine (Strattera), or
4) guanfacine (Intuniv, Tenex).
A child may do well on the first drug chosen. But often, one drug may have unwanted side-effects or weak benefits for that child. So then a different one of these drugs needs to be selected. Sometimes, the child benefits more from taking the drug twice per day. Depending upon other behavioral symptoms besides those of ADHD, some children receive a second medication, such as Clonidine (catapres), riperidone, or an anti-depressant.
Adult ADHD Outcomes
The recent German study published by Alexandra Philipsen, et al, in JAMA Psychiatry shows the same is true for adults with ADHD, adding medication produces more benefit than therapy alone. The researchers  analyzed data from 419 patients who had been randomly assigned to one of these four conditions: methylphenidate, individual therapy, structured cognitive behavioral group therapy, or placebo. Simply stated, the methylphenidate group experienced larger reductions in symptoms than patients in the two therapy conditions. The main measure was the ADHD Index of the Conners Adult ADHD Rating Scale.
analyzed data from 419 patients who had been randomly assigned to one of these four conditions: methylphenidate, individual therapy, structured cognitive behavioral group therapy, or placebo. Simply stated, the methylphenidate group experienced larger reductions in symptoms than patients in the two therapy conditions. The main measure was the ADHD Index of the Conners Adult ADHD Rating Scale.
The implications of these findings are of special importance for mental health professionals and ADHD patients.
- A reduction of 20-25% in symptoms can be achieved by a combination of therapy and medication.
- Medication should be added to the treatment regime in order to boost the improvement.
- Realistic expectations are important. The state-of-the-art approaches lead only to modest gains in ADHD symptoms.
The study only measured the overall ADHD Index on the Conners. (CAARS) Note that in addition to measuring how closely the patient’s symptoms match DSM-IV symptoms for ADHD, the Conners also measures various  other symptom domains as well. We present these in order to clarify that a person with ADHD has both SYMPTOMS, as measured in the study, and IMPAIRMENTS, that is, areas of functioning which are limited by ADHD symptoms.
other symptom domains as well. We present these in order to clarify that a person with ADHD has both SYMPTOMS, as measured in the study, and IMPAIRMENTS, that is, areas of functioning which are limited by ADHD symptoms.
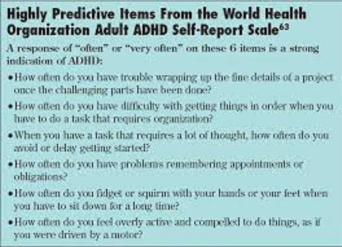
1) Inattention-Memory Problems – Since Working Memory deficits are thought to be central to ADHD, many patients have problems with concentration, short-term memory, forgetfulness, absent-mindedness, disorganization, and planning.
2) Hyperactivity/Restlessness – Many, but by no means all, patients feel or appear restless and have trouble sitting still.
3) Impulsivity/Emotional Lability – Many experience rapid shifts in mood (not to be confused with Bipolar Disorder), irritability, making snap choices without stopping to think about consequences.
4) Problems with Self-Concept – Lifelong difficulties with relationships, academic performance, and choices lead to a loss of self-esteem, a poor sense of competence.
The study did not determine if the treatments led to improvements in the  range of domains and impairments. Nor did the study look at long-term skill improvements specifically. However, since Conners scores did not go down much in the study overall, we see that, without medication, patients lagged in the acquisition of new skills.
range of domains and impairments. Nor did the study look at long-term skill improvements specifically. However, since Conners scores did not go down much in the study overall, we see that, without medication, patients lagged in the acquisition of new skills.
In recent years, an industry has arisen using coaching as an intervention with adults with ADHD. Motivated individuals can benefit from coaching or working with a psychotherapist to improve follow-through, completing important tasks, social interaction and relationships, and self-concept. The Philipsen study suggests that medication may enhance the ability to learn these crucial skills.
Lastly, ADHD is a lifelong condition. A person with ADHD learns
*to manage the symptoms
*to overcome the impairments,
*to acquire skills for effective performance in school, work, partnering, family life, and in the community
The study should not be read to mean that medication alone if the answer. Therapy or coaching is essential to helping many ADHD patients to manage the social, occupational, and educational effects of their primary ADHD symptoms.
*Click here to read the Sanja Gupta article.
Click here to read the abstract of the Philipsen article.
The entire article reference is:
Philipsen A, et al (2015). “Effects of group psychotherapy, individual counseling, methylphenidate, and placebo in the treatment of adult ADHD. JAMA Psychiatry, 2146.
If you have more interest in the Conners Adult ADHD Rating Scale (CAARS), here are two sites which give examples of scoring for the CAARS and a breakdown of the symptom domains measured by the Scale, which include the major areas of difficulty in adult ADHD. The scale itself is only available to trained mental health professionals.
CAARS: Long Version (CAARS-S:L)
CAARS: Short Version (CAARS-S:S)
If you want to dig deeper into the professional literature on Cognitive Behavioral Therapy for ADHD, a good place to start is this review:
Knouse, L.A., & Safren, S. (2010). Current Status of Cognitive Behavioral Therapy for Adult Attention-Deficit Hyperactivity Disorder. Psychiatric Clinics of North America, 33 #3, 497-50
This link to the Knouse and Safren article on PubMed brings the reader to a number of other articles on this subject:
Current Status of Cognitive Behavioral Therapy for Adult Attention-Deficit Hyperactivity Disorder