Therapy Gems ©
More on Buzz Words Versus Meaningful Words
Buzzwords II: Adding to Our Lexicon of Buzzwords, Psychobabble, and Vague Jargon
This article comments on more of the troubling buzzwords I have collected since my original article in 2012 (revised in 2017).
First, I want to acknowledge my staff. They quickly respond when I point out a buzzword during a case conference and universally they have cut most of these words out of our meetings. As a result, case presentations have more clarity and specificity. That leads to a higher quality of suggestions from the team.
The most frequent buzzwords seem to be “attention,” “acting out,” and the word “anger” used as a personal characteristic, as in “he has so much anger inside.” A brief, immediate explanation of the illogic of these terms has helped staff stop using them.
More Buzzwords
I have not come across many buzzwords that were not in my original paper on the subject. I do see some terms that I predict will become buzzwords or which are on the  cusp of buzz-word-dom. Here are some additional buzzwords or future buzzwords in mental health.
cusp of buzz-word-dom. Here are some additional buzzwords or future buzzwords in mental health.
Chemical imbalance — This term is the invention of drug marketers. It never had a scientific meaning! Imbalance between what chemicals? What kind of imbalance? Every benefit of a psychoactive medication is due to rectifying an imbalance?
It appears problems relate several factors, not to a question of imbalance – i.e., an excess of a chemical or a depletion of the chemical or too few receptor sites. If you have an excess of dopamine in some areas, which we believe has something to do with some symptoms, then you have an excess. Nothing is in or out of balance. If you have too few receptor sites for dopamine or serotonin, then you have too few receptor sites. If mono-amine oxidase breaks down mono-amines (nor-epinephrine, dopamine, serotonin), then that is the underlying process. There is no imbalance between dopamine and serotonin or between any other two neurotransmitters. There is no definable balance point.
The term was developed for the public as an obfuscating, easily acceptable, professional-sounding, generic explanation for why psychotropic medications may be valuable. Furthermore, research has not conclusively explained why many 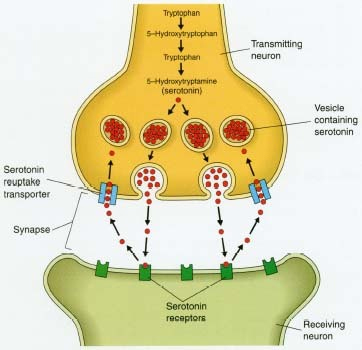 medications work or the degree to which some of them are actually effective. Nor has it validated some favorite hypotheses in the explanation of how chemicals work to reduce symptoms.
medications work or the degree to which some of them are actually effective. Nor has it validated some favorite hypotheses in the explanation of how chemicals work to reduce symptoms.
Unfortunately, this term has come to be reified. Consumers on psychiatric medications often think they have an imbalance. Using the metaphor of a chemical imbalance suggests a permanent feature of an individual. Sometimes the brain is in balance and sometimes not. In most cases, this is unlikely to be accurate an accurate reflection of the neuro-chemical status. The term also implies medications must be taken for a long time, which also may be doubtful, even for severe symptoms. The public has come to believe in medication for depression despite the fact that recent research shows about 80% of depressions are not helped by medications. Furthermore, research shows that psychotherapy alone is effect in a majority of cases, even with severe depressed mood.
Better would be to describe how some symptoms are reduced by certain medications, either without inferring process which we presently do not fully understand or with specifying the processes which we do understand. For example, an SSRI interferes with re-uptake of serotonin into neuron one so that neuron two fires, thereby increasing the intensity of signals in that mood-regulation pathway. If it is a pleasure, satisfaction, or affect regulating system, the person may feel calmer, more pleasant, or less unpleasant. Give the client the level of explanation that client wants, needs, or deserves. But give an honest account.
Co-dependent, co-dependence – When Melanie Beattie and others suggested this term, the meaning was narrow. Co-dependence refers to one type of relationship with someone who is dependent upon alcohol or drugs. To continue, despite the fact that he or she is not taking drugs, the co-dependent person also has a relationship to those chemicals, mediated by the behavior of the person who takes them. The co-dependent’s mood, thoughts, and actions are heavily structured around the patterns and behaviors of the person who is using the drugs. For instance, if one’s spouse uses cocaine, one may be resigned or furious, on the verge of leaving, considering giving the partner another chance or no more chances, sleepless when the partner is out on a binge, mistrustful, or endlessly checking up on the spouse. In other words, much of one’s mental process and behavior is taken up by the partner’s use. That is co-dependence. The term was meant to describe the state and behavior of a person who is in a relationship with another and that person’s drugs, a term more comprehensive than the earlier term “enabling.” In many ways, “enabling” can be a more specific term; it can be used to refer to one particular class of specific behaviors. “Co-dependent” can be so broad as to be confusing.
However, the term can be quite useful. But I seldom hear it being used correctly. I have heard a number of people say “co-dependent” when they merely mean “dependent” behavior. It reminds me of the linguistic conundrum of “regardless” becoming “irregardless.” I have heard it used to mean having a relationship with someone who uses, but by no means the complex relationship that the term originally described. So, I suggest the term only be used in its narrow sense or not at all. Or just describe the behavior.
Denial – I am listing denial with the buzzwords merely because the term is thrown around too easily and is now so popular that its original meaning is diluted. ‘Denial’  is often used to describe behavior such as rationalizing, minimizing, self-deception, failure to display insight, or refusing to be accountable for the impact of one’s actions. Denial may be used when the client continues in a self-destructive behavior despite negative consequences from the behavior by downplaying or refusing to accept that the behavior causes problems. Denial may get used as an accusation or criticism suggesting merely that the person using the word disagrees with the person in so-called denial. In other words, the term is thrown around too loosely. That is the very core of the genesis of buzzwords that grow out of professional jargon that originally had been useful.
is often used to describe behavior such as rationalizing, minimizing, self-deception, failure to display insight, or refusing to be accountable for the impact of one’s actions. Denial may be used when the client continues in a self-destructive behavior despite negative consequences from the behavior by downplaying or refusing to accept that the behavior causes problems. Denial may get used as an accusation or criticism suggesting merely that the person using the word disagrees with the person in so-called denial. In other words, the term is thrown around too loosely. That is the very core of the genesis of buzzwords that grow out of professional jargon that originally had been useful.
To use ‘denial’ correctly means going back to its roots when the term was used to describe an immature level defense mechanism in which one, in effect, distorts the perception or interpretation of reality so as to block awareness of the uncomfortable facts, memories, or impulses. Because the memory or feeling produces threat, anxiety, shame, or guilt, one does not want to acknowledge something is true. The process is unconscious. For instance, a person can see his father is drinking a lot, but he has powerful intrapsychic reasons to deny father is actually “an alcoholic.” It would feel threatening to one’s security to acknowledge it. A troubled child may be called merely rambunctious, which is a denial-by-minimizing of his aggressiveness, hyperactivity, and mischievousness.
The term also has multiple meanings even in a professional setting. One can “deny” that which is factual because of a) reality distortion, b) not wanting to talk about the subject due to anxiety, c) not wanting to admit the truth and accept the implications due to the threat involved in doing so, d) acting as if it’s not a problem or minimizing (usually because the implications of admitting the problem feel too threatening), e) evading accountability. In addition, f) one can accept facts, but deny having feelings about the situation. g) One can accept the behavior, but deny the behavior has negative consequences. For instance, “Sure I did hit him, but it’s not so bad. He deserved it and I didn’t leave any marks.” h) One can accept the behavior, but deny responsibility. “It was his fault!” i) One can try to explain or rationalize it away. “Johnny does it too, and I do it less than Johnny, so I don’t have a problem.” One can say, “I didn’t get it done, but the real reason I have this problem is Jill’s fault.” Each of these processes has a common factor, namely, the motivation is to avoid or escape from threat, anxiety, shame, or guilt.
Having so many meanings makes denial too easily thrown around as a catch-all term. The term also gets used as a form of confrontation and criticism.
I suggest the use of the term denial should always be followed by an explanation of the type of denial and a consideration of how the process is the client’s effort to preserve reality as he or she understands it. Words meant consciously to evade responsibility or justify one’s behavior are not denials and should be label more appropriately as rationalizations or justifications to avoid guilt, shame, punishment, or responsibility.

Energy — “Energy” has numerous meanings – enough so to make the use of the term in psychotherapy often strikingly imprecise. Let’s look at a few meanings both valid and questionable. I am not trying to be comprehensive, but rather to show the degree to which the word is a metaphor and how psychotherapists have started to use the term as a metaphor FOR a metaphor, a buzzword.
Freud used the term “psychic energy” to explain the flow of behavior from a presumed source – instinct or drive or wish – through the shaping of drive fulfillment by ego functions. In his approach, which aligned with mainstream concepts in  physics, behavior is motivated by internal sources, that is, it is driven by energies arising from drives. Freud was not alone in this concept of behavior. Indeed, many motivational theories of behavior in mainstream psychology in the early and middle 20th century began with concepts of drive or instinct. Since the body consumes energy (i.e., calories), it makes sense to consider, analogously, that energy operates in personality. However, such transfers of ideas from the operation of one system to another often lead to the realization that there is no one-to-one correspondence between systems. The mental system uses bodily energies (metabolism), but behavior seems to require far different explanations. For example, Watson and Skinner later showed behavior can be, in a sense, motivated by the perception (an internal function) of reinforcements. So the concept of psychic energy, which was inferential, metaphoric, and unmeasurable in the first place, fell out of favor.
physics, behavior is motivated by internal sources, that is, it is driven by energies arising from drives. Freud was not alone in this concept of behavior. Indeed, many motivational theories of behavior in mainstream psychology in the early and middle 20th century began with concepts of drive or instinct. Since the body consumes energy (i.e., calories), it makes sense to consider, analogously, that energy operates in personality. However, such transfers of ideas from the operation of one system to another often lead to the realization that there is no one-to-one correspondence between systems. The mental system uses bodily energies (metabolism), but behavior seems to require far different explanations. For example, Watson and Skinner later showed behavior can be, in a sense, motivated by the perception (an internal function) of reinforcements. So the concept of psychic energy, which was inferential, metaphoric, and unmeasurable in the first place, fell out of favor.
More recently, a number of psychotherapies accept categorization under “Energy Psychology.” These approaches accept the Chinese theory behind acupuncture, yoga, qi gong, etc., namely, that the body includes energy fields which may be blocked or functioning inadequately. Therefore, methods, such as inserting needles along “meridians” or exercises which affect “chakras,” lead to healing, perhaps by unblocking channels and releasing energy. Thought Field Therapy and Emotional Freedom Technique, popularly known as “tapping,” are energy psychologies. These approaches, hose mechanism of action is uncertain, overlap well-proven methods, such as “exposure” and “mindfulness.” To call them “energy psychology” is to use a metaphor. No energy can be found or proven.
In the vernacular, “energy” has a variety of figurative meanings besides the physical meaning of power (mechanical), heat (thermal), or quanta (nuclear).
- Energy refers to power, either potential power or kinetic power. So an act can express this power or vigor, either physically or, often, metaphorically, such as “He plays the game with high energy.” “His delivery of the speech was done with high energy.”
- A more metaphoric use of the word is contained in the idea of working off energy, where energy means something akin to tension.
- “Emotional energy” can mean a trait, something akin to get-up-and-go, outgoing personality, or personal activation. The level of energy can refer to a trait in the sense of referring to someone whose arousal and speed of activity is characteristically high or low in presumed energy.
- “Emotional energy” could also mean mood, such as “After the bad news, the room was drained of energy.” The meaning is one of inhibition, heavy-heartedness.
- “High energy” or “low energy” refers to arousal, wakefulness, or a related quality of mood. This meaning can refer to a state, as it is most commonly. “I don’t have the energy for that climb” means a state of lacking the activation for the task.
- Energy can be used to represent a passion or focus as in “He devoted his energy to writing.” Referring in a word to concepts of commitment, expenditure of time, and execution of tasks this use has little to do with the notion of physical energy per se.
Anyone using any of the above meanings probably can be understood clearly by most of us. We can tell from the context whether you mean vigor, power, high level of activity, forcefulness, nervousness, tension, mood level, extroversion, wakefulness, or focus.
But therapists often use “energy” in more ambiguous ways that we should avoid. For example, I have heard this sentence, “I sense your energy.” Not believing in auras, I find this kind of statement so vague as to be muddling.
In another example, I have heard this sentence, “You are full of negative energy. Your negative energy brings me down.” The reference is not energy at all. It could mean dead-end thinking, criticism, finding the problems in any advice, rumination, or other kind of negativity, all of which are subsumed under “negativism.” If that is what the therapist means, then be precise and give the process an accurate name.
In another example, we often hear, “I like your energy.” I don’t think that is meant to refer to any version of force or power. It is meant to refer to positive personality, enjoyable personality, or getting things done, or any number of positive qualities. That range of meaning alone makes the idea impossibly ambiguous.
In these three above examples, the word “energy” is used to mean something entirely other than energy!
Therapist should be more precise. If referring to energy in the Freudian sense, refer to “psychic energy.” If referring to Energy Psychology, in which the theory is unproven and the results could be attributed to well-known psychological process without reference to “energy” at all, I suggest referring to an “exercise” that helps the way acupuncture does. If using energy to mean one of the usual vernacular meanings, one of the synonyms that convey a meaning closer to what you intend probably will be more appropriate. But the very metaphoric, vague uses should be avoided. 
Evidence-based — How could such an important term be a buzzword? Simple. It is very easy to claim one’s treatment to be evidence-based, but it is very hard to demonstrate. Marketers and brochure-writers put the term into healthcare ads and brochures. Is that a guarantee? No. The term is now used as a seal of approval. But it is an over-simplification.
In reality, few mental health patients can simply receive an proven protocol – they are too complex. Also, many therapeutic efforts are given a name but lack faithfulness to the evidence based therapy. I frequently see a therapist name the therapy they are doing, giving it the name of a proven technique, but providing a method which is not very faithful to the method.
Let’s look briefly at this term. The term is supposed to refer to therapies for which controlled clinical trials have shown the therapy is better than placebo, wait list, another treatment, or no treatment at all. The term can be used to refer to meta-analyses showing the treatment has a reasonably strong effect size, roughly an average standard deviation between the treatment group and the control group of .4 or above.
Furthermore, a number of sets of guidelines have been published which incorporate such treatments, among them the Expert Consensus Guideline Series, guidelines by the American Association for Child and Adolescent Psychiatry, and guidelines from the American Psychiatric Association. Most payers have published guidelines as well.
But then reality always intrudes. Therapists vary in their awareness of the evidence. Therapists vary in their knowledge and training in such therapies. They vary in their adherence to these models. Clients in practice are usually more complex than subjects in trials.
Further, techniques do not account for the major share of the variance in outcomes. Relationship factors including the therapeutic alliance, empathy, and non-specific factors, such as hope, account for more of the variance.
Clients may not accept or want a recommended treatment. Often, other treatment functions must come first, such as stabilization, building resources, developing trust, or managing crises. So we may say we do evidence-based care, but in reality often we are not providing that care. The professional’s recommendation may not be evidentiary practice but may nonetheless reflect very good clinical judgment.
Another problem is that therapy can be narrow or broad, focused on one symptom or focused on a broad range of client functions. Some therapies are broad and generic, such as solution focused or psychoanalytic. Some are narrowly focused, such as systematic desensitization, EMDR, exposure, and specific protocols within the CBT world. There is no specific proven technique for many conditions. Harm Reduction, support, and directive counseling are often the main techniques one can offer where no treatment is proven to help.
Often the proven treatment is the wrong treatment for a particular client at a particular time. For example, a patient I’ll call Vicki came to treatment with a major depressive disorder. But rather than cognitive behavior therapy or interpersonal therapy, two proven methods, the therapist judged that the best choices to initiate were medication and crisis psychotherapy. Cognitive therapy was added after 6 crisis sessions. The relief produced by the initial plan led to successful completion of the case in 10 weeks without much use of the “proven” methods.
Often, clinical trials are sometimes not the same as real world situations and would eliminate patients such as Vicki. They compare “pure” diagnostic entities, which are not the same as the usual client seen in the clinic. Clinical trials eliminate patients with complex lives and multiple problems. When we work with complex cases, complex decisions have to be made which may belie the so-called evidence.
Many therapists depend upon clinical experience and clinical wisdom, often rightly. Treatment is so complex and difficult and problems are so complex that evidence-based treatments often have to wait until other care is provided in the real world. Published care guidelines developed by insurance companies may take economic factors too much into consideration, possibly weighing benefit plan structures against optimal treatments.
How good is the evidence? One critique showed that depression treatment by CBT is more lasting and in the long run more cost effective than medication. Another showed the so-called evidenced-based use of anti-depressants was no evidence at all – 80% of the cases did not need the medication.
Our comprehension of the evidence changes over time. From the 1950s declaration that therapy is no better than spontaneous recovery to the 1970s declaration that all therapists are about equally useful to now, the evidence changes and new therapies are constantly in development. We can assert that there are more proven approaches now. There are also more types of evidentiary approaches for specific problems.
Based upon cost-benefit considerations, EBT has a political and ideological agenda itself. Consider the case of PSA and mammograms – cost-benefit says to do one thing, clinical judgment another, patient safety another. The final criteria are somewhat ideological. We find the same biases in trauma treatment. Prolonged exposure therapy appears to have more of a following in academic psychology while EMDR, which produces equivalent results more quickly, may be downplayed by academics, but may be preferred by non-academic clinicians.
In conclusion, I prefer to use the term Evidence-Informed. This term acknowledges the research and the effective approaches, but with the understanding they must be provided within the larger overall context of the client’s treatment needs and the clinician’s best judgment.
I can’t breathe. You’re smothering me. — Such terms are not actually buzzwords; but they function as buzzwords. The client may mean, among many possibilities, that she feels controlled, her partner demands too much for her, she has no time alone, she uncomfortable in a close attachment, she feels her partner needs to be too close for her own comfort, or she is frightened of a relationship. “I can’t breathe” can also mean the opposite, namely, “I cane so much it takes my breath away.” Which is it? What’s the history behind the dynamic? How is it being repeated in her life? For the client, the term obscures the underlying emotion and memories. For the therapist, the meaning is too generic to be helpful. So the term does work like a buzzword – it tells us something we can only partially grasp and we need to ask for much more detail.
Hyper – What comes to mind with “hyper” could be restless, keyed-up, agitated, hyperactive and moving around the room or climbing on the furniture, “bouncing off the walls, anxious, over-stimulated, or hypo-manic. Furthermore, when used to describe a client, the word is more of a pejorative adjective than it is informative. As with many buzzwords, its effect is one of judgment and distancing. If we mean hyperactivity, we should say so. “Child was hyperactive, changing positions on the chair many times over 10 minutes, walking about the room investigating objects in the room, playing with an object briefly before moving to the next one.” If we mean agitated or anxious, we should use those more specific words.
Manic – For this buzzword, I know I am to a degree splitting hairs. But for professionals, we should speak clearly and use language carefully. When used to describe a true manic episode, “manic” is, of course, the proper word. “Manic’ may describe the mood of a manic episode, and doing so with a bipolar patient is entirely appropriate. 
I asked a team of clinicians what they might mean by “manic” and the terms they cited include agitated, excitable, high speed, hyper, keyed-up, on edge, restless energy, and tense. When used to describe the mood of a person who does not have a bipolar disorder, the description of that mood little resembles true mania per se. Using “manic” merely to describe mood does no justice to the experience of the bipolar patient. It does not describe the extreme, impairing severity of that mood, the racing thoughts, sleep disturbance, compromised judgment, inappropriate choices, extremes of irritability, and altered sense of self which characterize mania. In that case, calling a mood manic is a disservice to those who have bipolar disorder.
Move on, Moving on — Similar to “let go,” “move on” is meant to admonish someone to stop focusing on or talking about some troubling event or situation. “I need to move on” is an acknowledgment of a need to resolve a conflict or situation. People refer to ‘moved on’ in the past tense or ‘moving on’ as if they had accomplished a major step in life. Somehow, when someone claims to have moved on, I become skeptical. Have they emotionally resolved the loss or trouble? Or only worked on ignoring or repressing recall of it? To resolve a painful experience is to reach a psychological point at which the event feels historical rather than current and has the same emotional valance as almost any historically significant event, but no more than that.
The command to “move on” implies no such accomplishment. How is one to  accomplish it? Where does one start? What if one cannot move on; is that a failure? The term should not be used. The processes of grief work for a loss or of resolution of an emotional conflict or emotionally troubling experience are so rich with possibilities that it is imperative that we specify the processes. We should guide the client through a process. We should not be telling anyone to “move on.”
accomplish it? Where does one start? What if one cannot move on; is that a failure? The term should not be used. The processes of grief work for a loss or of resolution of an emotional conflict or emotionally troubling experience are so rich with possibilities that it is imperative that we specify the processes. We should guide the client through a process. We should not be telling anyone to “move on.”
People Pleaser — This term has always been a buzzword. It could be used to describe a passive or compliant person who is taken advantage of. It could be used to describe a peace-maker or a conflict-avoidant person who reduces negative emotional situations by offering solutions, usually ones in which she volunteers to take on a responsibility others should be taking on. It could mean someone has difficulty saying “No” and takes on too many tasks. It could mean a person who goes along with others rather than asserting a contrary position. This person has conflicts over self-assertion, over telling others she can’t or doesn’t want to do something. She may not ask for what she wants or needs. This person may present a false self to the world as someone unfailingly agreeable. She may compromise
others should be taking on. It could mean someone has difficulty saying “No” and takes on too many tasks. It could mean a person who goes along with others rather than asserting a contrary position. This person has conflicts over self-assertion, over telling others she can’t or doesn’t want to do something. She may not ask for what she wants or needs. This person may present a false self to the world as someone unfailingly agreeable. She may compromise  her position or wants so as to avoid conflict. Her self-worth may depend upon the approval of others. She may feel responsible for how others feel and may fear others being angry or disappointed in her. She may not trust her own perceptions and feelings, so she hides or discounts them. She may enable misbehavior in others and may be miserable about the result. She may need to be perceived as helpful, and never as lazy. The term could also mean a kindly person who truly enjoys doing for others.
her position or wants so as to avoid conflict. Her self-worth may depend upon the approval of others. She may feel responsible for how others feel and may fear others being angry or disappointed in her. She may not trust her own perceptions and feelings, so she hides or discounts them. She may enable misbehavior in others and may be miserable about the result. She may need to be perceived as helpful, and never as lazy. The term could also mean a kindly person who truly enjoys doing for others.
So which is it? As a term used in therapy, it has so many possible meanings that it lacks meaning. Is this person supposed to become more assertive? Or is she to work through her fear of alienating loved ones? Or her fear of loss? Or her early training that assertiveness will be punished? She can’t quite work out how she is supposed to be different once she is called a “people pleaser.” But she can be helped to work through the dynamic behind her behavior.
Let’s also avoid synonyms, such as pushover or overly nice or patsy. If a person fits any of the dynamics I’ve described, explain the pattern and drop the label.
Resistance – Resistance was first defined by Freud. His German word, “Den Widerstand,” translates as push-back, resistance, opposition. The term defines a  process in which the client is anxious due to the awareness of uncomfortable or unacceptable impulses or painful memories, and that anxiety motivates defenses which aim to repress, block, or constrict awareness or expression of those impulses or memories in therapy. Then the person ‘resists’ expressing the feelings or memories in therapy. He or she may suddenly block, may edit comments, may suppress them, may change the subject, or may miss sessions. The pressure to resist can be primary – avoidance of anxiety – or secondary – meaning the client has reinforcements (secondary gains) for maintain symptoms. The fundamental techniques of psychoanalysis are analysis of transference and analysis of resistance.
process in which the client is anxious due to the awareness of uncomfortable or unacceptable impulses or painful memories, and that anxiety motivates defenses which aim to repress, block, or constrict awareness or expression of those impulses or memories in therapy. Then the person ‘resists’ expressing the feelings or memories in therapy. He or she may suddenly block, may edit comments, may suppress them, may change the subject, or may miss sessions. The pressure to resist can be primary – avoidance of anxiety – or secondary – meaning the client has reinforcements (secondary gains) for maintain symptoms. The fundamental techniques of psychoanalysis are analysis of transference and analysis of resistance.
More recently, the topic of resistance has been a focus in the field of Motivational Interviewing (MI). In MI, resistance is defined as statements of “sustain talk,” comments supporting dysfunction and arguing against change. Studies show that the frequency of sustain talk is directly in proportion to how much the therapist presses the client to change or confronts the client with statements about the client’s behavior.
“Resistance” can become a buzzword when it is used loosely or confrontively. “You are resisting.” If directly instructing people to change got them to change, therapists would be unnecessary. Much of the work of therapy is helping people change using techniques therapists spend years studying. Telling the person to change is quite different from helping the person understand his or her patterns of behavior and understanding the problems with continuing in current patterns. We know how challenging it can be to help people change over-learned, long-practiced patterns.
The most common loose use of “resistance” is to rationalize why the client has not  changed or why the client has missed sessions. In this case, the word is used as a blaming word. It obscures what may be problems in the therapeutic relationship, the therapeutic alliance, the client’s life challenges, the level of distress caused by symptoms, or more classic problems of resistance. As with most of the other professional terms in our buzz-word papers, we just want the terms used accurately and we want therapists to push themselves to find and understand the processes at work in the client and in the therapy.
changed or why the client has missed sessions. In this case, the word is used as a blaming word. It obscures what may be problems in the therapeutic relationship, the therapeutic alliance, the client’s life challenges, the level of distress caused by symptoms, or more classic problems of resistance. As with most of the other professional terms in our buzz-word papers, we just want the terms used accurately and we want therapists to push themselves to find and understand the processes at work in the client and in the therapy.
Self-medicate – This term is not yet a buzzword. Soon! It is used glibly to suggest that some dysfunctional, probably self-harmful behavior is motivated by the need to reduce or eliminate some emotion or discomfort. It is not meant to suggest a healthy medication used in the intended way for the intended purpose. Rather, it suggests the

Many people have come to believe we have a chemical solution for every problem or discomfort.
use of a medication in an inappropriate way or in a dosage exceeding the recommended dosage and for the purpose of altering negative mood. It also may mean a behavior, such as self-cutting or gambling, which has the effect of reducing some negative emotions. However, the term obscures the client’s significant difficulties managing the underlying emotions, the life history behind those emotions, and the history behind the difficulty coping with those feelings.
Furthermore, this term is used glibly; but often it may be incorrect. For example, the client may use the medication because the use has reached the point of dependency. So the use is not to self-medicate some underlying core psychological conflict, but rather to avoid withdrawal symptoms. Better would be to specify what underlying difficulty the client appears to be avoiding and the source of those difficulties. For example, “Due to PTSD, when the intrusive images flood his mind, he feels frightened and helpless. He discovered alprazolam calms his anxiety so he can function.” This explanation leads to interventions more effective than the term “self-medicate” conveys. “Self-medicate” leads mainly to confrontation and promoting abstinence. When we use a more specific explanation, we can see other possibilities, such as, affect management, trauma exposure therapies, or use of more appropriate medication.
Stuff It – This term is used to mean suppressing or trying to block the expression of negative emotions, such as feeling angry, frustrated, disappointed, scared, hurt, etc. The person may judge the expression of those feelings is unsafe, not tactful for the situation, or likely to be punished or dismissed. The closest professional term for this behavior is the defense of “suppression,” that is, purposeful restraint of the expression of a thought or feeling. “Inhibition,” “repression,” “dissociation,” “undoing,” and “emotional constriction” describe less conscious processes for blocking expression of emotion. That at least six psychological processes involve holding back or “stuffing” emotions demonstrates that the term “stuff it” or “stuffed my feelings” is vague, unworthy of expressing the richness behind these processes. The person may be afraid to express feelings or may be conflict-avoidant. To help someone, we cannot merely say “You are stuffing your feelings.” Nor should we accept the client saying, “I stuffed it so we wouldn’t fight over it.” Rather, we need to know the emotions, their source, and what experiences shaped the defense of suppression, repression, undoing, or whichever process may be present. We also need to be aware that suppression can be a healthy defense akin to tact. In that event, the pejorative term, “stuff it,” is just inappropriate.
Supportive – Supportive, as a buzzword, is a global term referring to no one set of well-defined of behaviors. Rather, one uses the feeling of “support” to mean the experience that the Other’s behavior FEELS accepting, validating, affirming, helping, or encouraging. When a person claims, “You are not supportive,” often the Other is not clear what behavior would produce such feelings or why his or her behaviors are not perceived as supporting. Often, the Other does not grasp the need to be supportive in a particular interaction and may perceive a different response is called for, perhaps a question or a practical suggestion. Let’s say one spouse says “You’re not supportive” and the other says “What do you mean?” or “I did [this and that] which I think was supportive.” The first is actually describing her experience, the feel of the spouse’s behavior. The Spouse, however, is describing his behavior. When I have encountered these interactions in couples counseling, it’s clear they are not discussing the same terrain.
To continue, a person may say, “You’re not supportive.” That is a judgment. A therapist might say, “You didn’t feel supported.” But the therapist should not empathize with a judgment as it condones that way of perceiving. But does that mean the client feels disappointed, alone, hurt, abandoned, invalidated, helpless, rejected, OR infuriated? In therapy, each possible emotion that is covered by the term “not supportive” leads FROM a different underlying dynamic and leads TO a somewhat different intervention. When the therapist accepts the term or the complaint of “not supportive” in a session without further clarification, he or she condones a surface view without deeper examination: it implicitly sides with the complainant. Thus, the interaction locates the client’s problem as external rather than as an examination of her need, her expression of her needs and wants, her history of relationships, or whatever other dynamic may be present. Nor does it lead to a closer examination of the therapist’s behavior that may have evoked the complaint.
Note, supportive does have some highly specific meanings which are not buzzwords. It can be used in an effective way, such as “I am supportive of your idea,” where supportive essentially means agreement or encouragement. Furthermore, it has been used for 100 years to mean Supportive Psychotherapy. That is an undefined set of interventions used in a crisis situation, with a patient who has weak ego strength, or with a psychotic patient. The interventions include empathy, using a calming voice, de-escalating situations, approaching the patient slowly, validating the patient’s point of view, patience, building trust, and highlighting the more effective defenses (e.g., intellectualization) and not reinforcing the less effective defenses (e.g., projection, acting out). It may mean temporarily accepting denial. It also mans avoiding confrontive or in-depth methods. So when a therapist refers to “supportive” interventions, that would be an appropriate use of the term.
More Future Buzzwords
These words still have a precise meaning to professionals. But in common usage they are becoming muddled. Some day they may be so imprecise that we will need to come up with new terms for the same phenomena.
Authentic – Carl Rogers defined ‘authenticity’ as the therapist’s full awareness and acceptance of his or her emotions and as communicating empathy sincerely (rather than formulaically). Optimally, we want the client to achieve this same state of awareness. By being authentic, therapists can be more empathic and can better discriminate reality from client transferences.
Now the word is on the move! I have heard it used as a positive trait, as in, “I am being an authentic person.” I’ve heard it refer to a positive state, as in, “I am being authentic with you.” As a defect, “You don’t know how to be authentic.” As a failing or accusation, “You are not being authentic.” Such claims and criticisms belie the fact that, in ordinary conversation, authenticity is often far from useful. For many situations in daily life, tact is more crucial than is total emotional honesty. Total honesty can be used as a form of aggression. If the opposite of authentic is tactful, acting, or playing a role while hiding one’s self, then often social effectiveness often calls for these niceties of behavior.
Finally, authenticity implies we know our feelings or thoughts in a situation; but we often have complex or even contradictory feelings and reactions. We do not want to dissemble or to be inauthentic, so what one says should be sincere and valid. Outside of the behavior of therapists working with clients, we would be okay if we left it to mean an optimal or goal state rather than requirement. Because the word is not all that widely used, it may not make it to buzzword status.
Bipolar, Mood Swings – Popularity may undermine the use of these terms. In common parlance, people are using bipolar to describe mood swings which are unexpectedly large and not immediately comprehensible. Others use bipolar as if it were a trait, as in “My bipolar,” not because the person has Bipolar Disorder, but merely as a description of mood swings or even as an explanation or excuse for mood-driven actions. “I’m sorry. It was my bipolar tendency that caused me to lose my temper.”
parlance, people are using bipolar to describe mood swings which are unexpectedly large and not immediately comprehensible. Others use bipolar as if it were a trait, as in “My bipolar,” not because the person has Bipolar Disorder, but merely as a description of mood swings or even as an explanation or excuse for mood-driven actions. “I’m sorry. It was my bipolar tendency that caused me to lose my temper.”
Mood swings, as thought of by professionals, mean highly significant shifts in mood. So on a -5 (despair) to +5 (joy) scale or a -5 (raging) to +5 scale (calm, accepting), professionals use mood swings more or less to mean -4 to +4 or the reverse. But in common usage, I hear mood swings used to describe any undesirable or rapid shift, as, for instance, when a person who is irritable and shifts from -2 to 0 or +1 – not a clinically significant shift.
Professionals may be contributing to this trend. The diagnosis of Bipolar Disorder may be, shall I say, sometimes in the category of a kind of fad, a term too easily applied, too many false positives. I have three male clients, each of whom has been diagnosed as having bipolar disorder. Since I have had the opportunity to spend many hours working with these men, I can say with some assurance that none have Bipolar  Disorder and so mood stabilizing medications used for true Bipolar have not helped them. Two of these men have symptoms of Major Depressive Disorder, Recurring, Chronic, without intra-episode remission.
Disorder and so mood stabilizing medications used for true Bipolar have not helped them. Two of these men have symptoms of Major Depressive Disorder, Recurring, Chronic, without intra-episode remission.
One of them was diagnosed as Bipolar at a time when he was drinking too heavily, combined with taking (prescribed) benzodiazepines, and while also being subject to seizures. Another was diagnosed as Bipolar on the strength of a couple of questions during an outpatient psychiatry visit. His MDD was determined to be Bipolar II. He told me he was asked, “Have you even had a time when your mood was overly positive, so much so you had high energy and didn’t need to sleep as much?” He answered in the affirmative, not because this positive mood was frequent or prolonged, but only because he had fleeting moments of those feelings. He was given Depakote, but he reported no change in mood.
The third man was diagnosed as Bipolar, but when I took a careful history and asked, as I always do, about gambling problems, he reported a period of severe pathological gambling. That was when he received the Bipolar diagnosis. Questions about typical behavior in heavy gamblers showed all the so-called “bipolar” behaviors were related to gambling, including not needing sleep, mood swings, irritability, and periods of euphoria. When I saw him, his gambling problem was in remission and I found nothing more serious than a problem of Adjustment Disorder with Depressed Mood due to events related to a divorce.
These stories are three of a number of times my trainees or I questioned the client’s diagnosis of Bipolar Disorder, especially when the diagnosis was given to youth 10-18 during a crisis situation in an inpatient setting. [Just to be fair, the criteria for Bipolar were met in the majority of cases in which the diagnosis was given. Further, there were some false negatives, meaning cases not given the Bipolar diagnosis who probably should have been.] My point here is that inaccurate usage by professionals contributes to the imprecise use of the term by the public, and some day “Bipolar” may become a buzz word as a result.
OCD, Obsessive Compulsive – I have heard “OCD” used as an adjective without the  speaker intending to refer to ICD-10 or DSM-5 definitions of OCD, as in “That was awfully OCD of you,” meaning, highly organized or persnickety. Many people have very minor impulses towards checking behavior, which, when severe, is a sign of OCD. Many people have very minor needs to create symmetry or to be overly concerned about odd and even numbers, or some other fairly trivial compulsion. I say minor in that, unlike a person with OCD, the behavior does not dominate the person. The person can check just once that she locked the car and then will be satisfied. In contrast, the person with OCD may have a ritual number of times to check and spends considerable time checking and re-checking when he or she performed the behavior. True OCD is a problem which can dominate a life. As with Bipolar, OCD can be used to explain or excuse behavior. It can be used as a complaint or criticism. We professionals should use the term with care to use it accurately.
speaker intending to refer to ICD-10 or DSM-5 definitions of OCD, as in “That was awfully OCD of you,” meaning, highly organized or persnickety. Many people have very minor impulses towards checking behavior, which, when severe, is a sign of OCD. Many people have very minor needs to create symmetry or to be overly concerned about odd and even numbers, or some other fairly trivial compulsion. I say minor in that, unlike a person with OCD, the behavior does not dominate the person. The person can check just once that she locked the car and then will be satisfied. In contrast, the person with OCD may have a ritual number of times to check and spends considerable time checking and re-checking when he or she performed the behavior. True OCD is a problem which can dominate a life. As with Bipolar, OCD can be used to explain or excuse behavior. It can be used as a complaint or criticism. We professionals should use the term with care to use it accurately.
Professionals Using Labels for Methods
In the past couple of years, I have asked people interviewing for jobs at the post-Masters level (mostly recent grads) to describe the treatment approaches they favor. The most common answers are Cognitive Behavioral Therapy (CBT), Solution-Focused Brief Therapy (SFBT), and Motivational Interviewing (MI). You know by now that I want to know specifics. “What specific techniques in that approach have you been using most?” For CBT, not one person in a long sequence of applicants said
Much more than pointing out inaccurate, dysfunctional thoughts. Few labeled them “automatic thoughts” or “core beliefs.” None identified a single behavioral method within CBT. None used measurement tools or thought experiments.
If the person mentioned SFBT, he or she didn’t tend to grasp the underlying  philosophy that the client has the solutions and we can elicit and amplify them. None understood the idea of exceptions or the importance of subtlety in the use of language. What many described seemed more problem-focused or more directive in the search for solutions to problems. A few could reference the “miracle question,” but not its significance in a process.
philosophy that the client has the solutions and we can elicit and amplify them. None understood the idea of exceptions or the importance of subtlety in the use of language. What many described seemed more problem-focused or more directive in the search for solutions to problems. A few could reference the “miracle question,” but not its significance in a process.
As for MI, most gave answers inconsistent with the philosophy of empathic guiding. Their concept of MI was rather directive and involved making sure to point to consequences of the behavior.
This is not to indict schools or internships. Well, not severely, anyway. But rather I am making the same point as with buzzwords. Our role is to be precise and clear. If one uses a term, know what it means. If one knows about a therapy, be able to describe its theory of problems and pathology, its principles of change, and its major interventions. MI is a form of intervention, not a therapy per se, which posits that much of what is termed “resistance” or “denial” is “sustain talk,” often induced by therapists putting pressure on the individual to change. If one claims to know this intervention, know what MI research shows to be the factors which reduce or which increase motivation to change.
This difficulty explaining therapies is not limited to new graduates. Many therapists have difficulty explaining the theoretical rationale for interventions or the breadth of concepts in a school of therapy. My point in presenting these observations is to highlight the tendency to use terms imprecisely until they have lost specificity of meaning. Therapists should be careful to use words accurately.
The third paper in this series on buzzwords unpacks our tendency to use buzzwords. I suppose that people who came for interviews had some of the motivations I examine in that paper. They may have been trying to convey a sense of status, of being part of the in-crowd, or of being highly knowledgeable. They may have been using terminology they picked up in school or at an internship. Regardless, they conveyed the opposite – lack of understanding and shallowness of thought. Furthermore, when we use the name of a therapy loosely, we lose the power to explain what we are doing. If we cannot explain, we cannot select treatments thoughtfully.
In written documents, avoid buzzwords. At the worst, the reader may perceive both the imprecision of meaning and a pejorative tone in the words. Don’t use buzzwords in notes, reports, or letters. The purpose of a document is to provide professional clinical assessment and judgment. The document is meant to communicate to other professionals. So it must be accurate.
In conclusion, in two papers, I have explicated a number of buzzwords and words that are heading toward becoming buzzwords.
- Acting out
- Anal
- Attention, Attention seeking
- Attitude
- Authentic
- Bipolar
- Can’t stand it
- Chemical imbalance
- Closure
- Co-dependence
- Deal with it, Can’t deal with it
- Denial
- Empower
- Energy
- Evidence-based
- Feel
- Fight
- Handle it, can’t handle it
- Hyper
- I can’t breathe, you’re smothering me
- Issue
- Let go, letting go
- Listen
- Manic
- Move on
- OCD
- Over-reacting
- People pleaser
- Process, processed’
- Resisting, resistance
- Respect
- Self-medicate
- Shut down
- Space, need space
- Stuff it
- Support
We’ll keep our eyes and ears open for precision in language and understanding. We can highlight and reinforce such accuracy in thinking.  We’ll keep our eyes and ears open for imprecise, vague language and work to improve it.
We’ll keep our eyes and ears open for imprecise, vague language and work to improve it.
************************
© Don D Rosenberg, Version 1.0 2017